Why we need to listen to our bowel symptoms
So many young women have approached me about endometriosis – and its related symptoms – to help determine if they have the disease. Because of their age, the vast majority have been told by their doctors that it is likely they have endometriosis but it has not been confirmed through laparoscopy – the only way to confirm endometriosis today. In almost all cases, however, the number one symptom that is consistent with all these young women I have spoken to is increased diarrhea during menstruation.
Over 90% of women diagnosed with endometriosis actually present with GI symptoms as their initial symptoms. Bloating is the most common presenting symptom, and is typically reported by 83% of women with endometriosis” – Lagyndr.com
Not only is this so common, it is a leading factor in misdiagnosing these women with either IBS before the diagnosis of endometriosis has been made. But why is that? Why do we poop more during our periods? Why arent doctors being more diligent in finding the right cause?
OK lets start with ovulation…
Estrogen and progesterone – both naturally occurring hormones in the body – play a role in reproduction (aka sex hormones). Leading up to your period, during ovulation, estrogen is at its peak levels to stimulate the release of an egg. “From then on, oestrogen levels begin to fall. Meanwhile, after ovulation, progesterone does the opposite of oestrogen and continues to rise; this is in order to prepare your womb for the fertilisation of your egg.” – Emma Thornton.
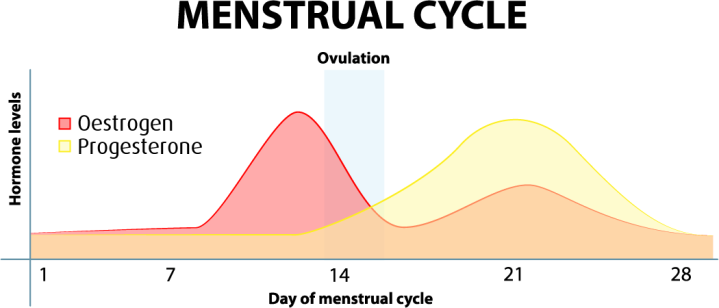
Progesterone can typically cause a bit of constipation but when levels of progesterone are depleted so quickly toward these last two weeks it can release its constipating effects and as result can stimulate some diarrhea (or rather, increased gut motility). While most women between the age of 18-40 are on birth control to help with the pain, the levels of these hormones are usually not as controlled in women with endometriosis and thus symptoms like cramping and diarrhea still break through.
Then you start bleeding…
It has been shown that cramping associated with menstruation is linked to prostaglandins – a hormone-like substance found in the tissue that are signaled to contract to facilitate the shedding of your lining (thus your period). Unfortunately, prostaglandins are found in basically any tissue that is able to contract (aka inflammation) and therefore when the body sends signals for them to contract, it most likely also results in contraction of your bowels. We all know cramping of your bowels is a sure way to stimulate some poop. Note that “Higher levels of prostaglandins are associated with more-severe menstrual cramps” and these higher levels are associated with a number of possible hormone-related issues such as Endometriosis. For those of us who have endometriosis on other parts of our bodies such as our thoracic cavity, we also notice cramping there too. Ouch!
Now lets talk about the gut…
In parallel we know that estrogen hormone receptors are found within the gut. There are several different interactions between estrogen and the gut that we are just beginning to understand, one of which may be the interaction of estrogen with estrogen-metabolizing bacteria residing in the gut which may promote certain side effects such as bloating. Gut microbiota shifts (lower lactobacilli concentrations and higher Gram negative
bacteria levels) have been demonstrated in a primate study of endometriosis, although the mechanisms linking these remain unclear.
We also know that medications such as the well known drug Lupron work by blocking Gonadotropin. “Gonadotropin releasing hormone agonist (GnRHa) stimulates the
production of follicle-stimulating hormone and luteinizing hormone thereby suppressing estrogen production making it a common treatment for the estrogen-driven disease, endometriosis.” If you are not familiar with Lupron and other drugs that work by this mechanism, they put you into chemical menopause which results in a laundry list of potential side effects. However we have seen that by this mechanism – by suppressing estrogen production – certain symptoms such as diarrhea may become tolerable.
Now you talk to your doctor and the conversation goes like this…
“I have painful periods and with it I get a lot of diarrhea” – the doctor glazes over the part about your painful periods and goes right to the diarrhea. First thing, lets get you a colonoscopy to see if there is any inflammation in your colon. Dr. Ken Sinervo from the Center for Endometriosis provides a wealth of knowledge about this very topic here. In a nutshell “As many as 8% of endometriosis patients with bowel symptoms may eventually be diagnosed with inflammatory bowel disease. IBD is usually characterized by abdominal pain, constipation, diarrhea, or alternating bouts of constipation and diarrhea as well as intestinal cramping.” You may be saying this sounds like you but your doctor said they didnt find anything. IBD is very distinct when looking through a camera. The gastroenterologist can see particular parts of your lining (Ulcerative Colitis) or throughout layers of your bowel (Crohn’s Disease) that are massively inflamed from physical ulcers formed therein. If the gastroenterologist doesnt see this they may order a fecal test called fecal calprotectin, which will test for inflammation specific to the gut through a biomarker that can be found in your stool. If both come back negative, and your doctor is thorough, they may choose to monitor any subsequent flare ups by ordering recurring calprotectin tests and measure the potential escalation in inflammation.
But my doctor gave me antidepressants and shooed me away…
If your doctor doesnt know how to look for the signs of endometriosis or doesnt feel the need to put you through a colonoscopy they may diagnose you with something called IBS. IBS is very similar to IBD but in lieu of physical lacerations in your colon you have a faulty gut-brain signal which means your brain is sending your gut these signals to poop. Accordingly to Dr. Sinervo:
Irritable Bowel Syndrome (IBS) is usually treated with dietary changes to avoid food triggers, and increasing dietary fiber. In some patients, stress can be a trigger. Avoiding stress or learning to deal more effectively with stress may help reduce the number of episodes. Exercise is beneficial for many patients. Medications are necessary for some patients. These may include anti-depressants, anti-spasmodics and other medications. In addition, medications that work better for patients with predominantly diarrhea or constipation are also available and have been shown to be beneficial for some, but not all patients.
Lets get technical for a second…
Both IBD and IBS, while they have different signature features, affect the gut. The goal then is to slow down the gut motility – the speed at which food moves through your gut – to try to reduce the number of bowel movements you have in a day. One hot topic at the moment is the gut microbiome. Many women with endometriosis experience something called ‘endobelly’. People with IBS or IBD have similar bloating without the catchy name. If a food diary is kept on hand most patients will identify certain trigger foods that will result in massive bloating. TMI Alert: this bloating is not something you can fart out, it needs to be dissipated over time. Why does this happen?
There is a community of bacteria that live in your gut – known as your gut microbiome. The bacteria have been around since birth, and each person has a unique microbiome based on their diet, their environment, their immune system and a wealth of other factors. The important thing is that you want to keep your gut microbiome healthy, meaning you want to keep particular strains of bacteria in higher quantity – the ones that have a protective nature – and you want to keep other bacteria like sugar-loving bacteria low in population. Antibiotics are a sure way of killing both the good and the bad bacteria, which is why so many of us in the medical community are really against shotgun approaches that render the host (thats you!) without any defense. Nonetheless, after your doctor has guided you on some diet changes such as low fiber and perhaps to stay away from dairy and red meat (other foods that cause bloating and inflammation) you might notice that your bloating is controlled and your diarrhea is not so bad. This is great! Lets not knock it, but it doesnt mean you dont have endometriosis. It just means you are killing off the bad bacteria in your gut – the ones that feed off dairy and sugar and in turn cause massive bloating. These bacteria – if fed properly – would emit gases that cause your bloating. Not convinced? Try taking some capsules of activated charcoal when you are really bloated. The charcoal absorbs any gaseous toxins and removes them through your poop (your poop will be black from the charcoal), and in turn will relieve the bloating caused by these gases.
But the pain is back (or never left)…
If the dietary changes are working for you, stay on them. Because even if you do have endometriosis you will eventually want to adhere to what’s known as the ‘endo diet’ or the ‘inflammatory diet’ which is similar to what you have been doing: no dairy, red meat, or gluten. For those of you with diagnosed IBD, you can follow along in my journey converting from a low residue diet (full of rice, bread and pasta) to one that is low in gluten. But what about the pain? All of a sudden you have to scream for someone to listen to you because, while it’s great that you are not pooping ten times a day anymore, the period pain is still unbearable!
Unfortunately at this time the only way to diagnose endometriosis is through a laparoscopic surgery where they will take a biopsy of the tissue and will remove any endometriosis that can be found while they are inside of you. In Canada and many other countries you need to have had 1 year of failed pregnancy to be referred to a fertility clinic where they then assess your eggs, fallopian tubes and other hormonal factors. Putting the pieces together they can make a case for surgery to make an official diagnosis. For women who are too young to be trying to have a baby, or choose not to have a baby, you will need to be referred to an endometriosis specialist who may or may not want to operate right away but instead help with pain management until it is too unbearable. I know I am painting a very sad picture right now but this is the reality. And to be honest I don’t know the process in other countries.
The first step in pain management is birth control. I know…, they suck! But the reality is that getting your hormones in check will certainly help with the pain. You may need to experiment with a few different types of birth control to see which one fits you best. If estradiol-progestin birth controls dont mitigate the pain, the next step might be to try medications that only contain progestin. Reducing the estrogen content in your body by removing the chemical mimic (estradiol) might help with the pain as well. In fact, along with the progestin-only birth control they may suggest getting rid of your cycle altogether by taking the pill continuously. The hope is that by eliminating any spikes in estrogen which would occur during your cycle this would completely stop menstruation and any side effects that come along with it.
Now it’s time for surgery…
During the surgery you will be put under. The laparoscopic surgery makes three tiny holes in your abdomen and leaves very small scars. There is no telling where the doctors will find your endometriosis but the goal is to remove anything they can see. The point of me dragging this blog on for so long is because in a small percentage of women the endometriosis may be found on or around the bowel which may have contributed to the diarrhea in the first place. That contractile tissue we talked about earlier would have been contracting against your bowel which would have definitely produced some painful diarrhea.
When the endometrial tissue is gone all we can do is hope for the pain, cramping and pooping to be reduced and then we continue the journey from there. Part of the reality is having an official diagnosis which in some ways does bring a sigh of relief. Always looking at the positive 🙂
Please reach out if you have any questions!
One thought on “Periods and Poop”